What is this leaflet about?
This information leaflet will help you understand why we need to discuss your Body Mass Index (also called BMI) and what the implications of a high BMI might be for you and your baby.
We understand that it may be difficult for you to talk about your weight but hope to reassure you that all health professionals will be sensitive towards you. We do however, need to make you aware of the risks associated with a high BMI in pregnancy.
If you have any questions or concerns, please speak to your midwife or obstetric team.
Is my BMI high?
Your BMI at the beginning of your pregnancy is a useful way to find out if you are a healthy weight. BMI is a comparison of your height and weight.
If your BMI is:
18.5 - 24.9 You are a healthy weight.
25 - 29.9 You are classed as being overweight.
Above 30 You are classed as being obese.
If your BMI is greater than 35, you fall into a category of women who are at a greater risk in pregnancy, birth and the postnatal period.
Increased weight puts you at greater risk of developing some medical complications during your pregnancy. These may include:
- Miscarriage, stillbirth and birth defects (such as neural tube defects).
- High blood pressure or pre-eclampsia. BMI over 30 increases your risk of pre-eclampsia by 2-4 times compared to a BMI under 25. This means you should have your blood pressure and urine checked at every antenatal visit.
- Diabetes in pregnancy (gestational diabetes). A glucose tolerance test (GTT) will be encouraged when you are 26-28 weeks pregnant, to assess if you have developed this condition. This is a blood test.
- Blood clots in your leg or lung blood vessels (thrombosis), which can lead to serious complications. You will be assessed for your risk of thrombosis throughout your pregnancy. You may need to be given blood thinning injections after the birth of your baby to prevent this from happening, depending on your BMI, your general health and how you gave birth.
- Ultrasound scanning may be difficult, and we may not be able to obtain clear images of your baby. This not only limits our ability to accurately diagnose problems but greatly increases the chances of significant problems not being detected at all by scan. It may also be difficult to assess your baby’s growth accurately.
You may have a higher likelihood of experiencing some problems in labour. These may include:
- Having a longer than average labour.
- Baby being born before 37 weeks.
- Having a higher chance of needing a Caesarean section and subsequent wound infection.
- Higher risk of heavy bleeding after the baby is born.
- It can be difficult and sometimes not possible to give you an epidural or spinal if you have a high BMI. There can also be problems with general anaesthesia during and after the operation.
- You may also be offered a cannula in early labour.
- Large baby
- Birth injury including shoulder dystocia (difficulty delivering the baby’s shoulders)
- Placental insufficiency
- Birth defects such as neural tube defects (defects of the brain and spinal cord).
- Difficulty monitoring baby’s heartbeat during labour
- Obesity in later life
- Admission to special care
- Your midwife will discuss the importance of exercise and eating a balanced diet during your pregnancy at your initial booking appointment. If you live in Warwickshire, you may be eligible for weight management services, please speak to your midwife about this.
- If your BMI is over 30 it is advised to gain no more than 9kgs during the pregnancy, as excessive weight can further increase the risk of complications
- You will be advised to take folic acid daily for the first 12 completed weeks of pregnancy, to reduce the risk of neural tube defects (defects of the brain and spinal cord). This will need to be prescribed as early as possible in the pregnancy.
- You will be advised to take Vitamin D daily, until the end of pregnancy. If you choose to breastfeed, we would recommend you continue to take Vitamin D post-delivery. Vitamin D helps to keep your bones and teeth healthy.
- You may need to take Aspirin daily from 12 weeks of pregnancy. The obstetric team will advise you if this is necessary.
- You will be re-weighed at antenatal appointments.
- You will be offered an appointment for a Glucose Tolerance Test between 26-28 weeks of pregnancy.
- If your BMI is greater than 35, you will be booked for extra scans to monitor baby's growth.
- You will see a doctor during pregnancy, usually in line with your scans. They will make a personalised care plan for you throughout your pregnancy and discuss place of birth.
- If your BMI is greater than 45, you will be offered an appointment with a Consultant Anaesthetist. This will allow you to be examined before your due date and discuss and plan pain relief and anaesthetic choices for your labour and delivery.
- You may sometimes need a course of blood thinning injections (Enoxaparin) throughout the pregnancy; this is to reduce the risk of you developing blood clots.
Your weight will increase because of the weight of the baby and placenta, as well as extra body fluid, blood, fat stores and tissue your body builds to protect baby. Generally, this adds up to around 14lbs but this can vary from individual to individual.
Currently, Institute of Medicine guidelines recommend a pregnancy weight gain of:
BMI over 25 = 7-11kgs (15-25lbs)
BMI over 30 = 5-9kgs (11-20lbs)
If you would like help and advice on weight management in pregnancy, ask your GP or midwife who can refer you to a dietician.
Weight loss and dieting is not recommended in pregnancy, but it is best to try and control weight gain. This can be done by:
- Portion control.
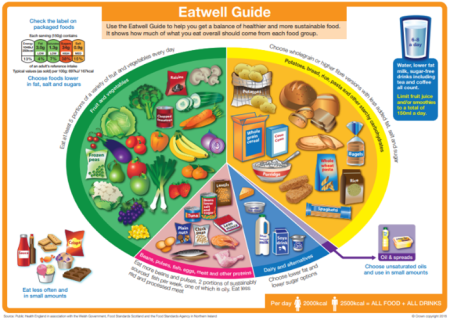
- Ensuring you are maintaining a healthy diet following the “eat well plate”
- Steadily increasing movement in pregnancy. It is recommended that pregnant women complete 150 minutes of low or moderate exercise per week.
Movement can be increased by opting to take the stairs over the escalator or lift. Swimming, yoga and walking are all good options. Walking is one of the easiest ways to fit activity into a busy life. Any form of movement is great, such as gardening or cleaning the house.
It is recommended that those with a previously sedentary lifestyle commence with 15 minutes of activity 3 times per week and gradually increase this over time to build up to 150 minutes. Moderate exercise is anything that increases your heart rate and breathing but where you are still able to hold a conversation.
Please note any form of activity counts and can be broken down into shorter 10 minute bouts of exercise. You should still be able to maintain a conversation when exercising.
Those who are active can continue with the same activity level, but the type of activity may need to be changed, for example: avoiding contact sports or high-risk activities such as skiing, surfing, horse riding and diving.
*please note: avoid laying on your back after 1st trimester due to risk of reduced cardiac output and this can cause you to feel faint*
Avoiding excessive weight gain might help you to:
- Have a more comfortable and enjoyable pregnancy, be more mobile and less likely to suffer with pelvic pain.
- Have less weight to lose after you have had your baby. It could also reduce the risk of your baby developing obesity during later life.
- Reduce the risk of pregnancy complications.
Nutrition is very important during pregnancy. The Eatwell Guide will help guide you on the food groups you need to consume to keep healthy and the proportions of each food group. This can be found here: https://
Eating healthily during pregnancy will help your baby to grow and develop and will help you to keep well. It is important to eat a variety of different foods to get the right balance of nutrients and vitamins and minerals you need.
It is a myth that you should eat for two in pregnancy, as the baby will take everything he/she needs from your body. You only require an extra 200 calories in the last 3 months of pregnancy. This is the equivalent of 2 slices of toast!
Suggestions:
- Try and swap out unhealthy snacks such as crisps, chocolate, cakes and fizzy drinks for dried fruit such as apricots and raisins, hummus and vegetable sticks, yoghurts, rice cakes and unsweetened breakfast cereals.
- Try not to skip breakfast as eating breakfast can help keep you fuller during the day.
- Avoid eating large portions.
- Aim to steam, bake or grill your food and avoid adding extra fat.
- Eat wholemeal and low sugar versions of foods where appropriate.
Information about what you can and cannot eat in pregnancy can be confusing. Below is a simple table that illustrates what is safe and what is not!
| EAT | AVOID |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Pregnancy and having a baby is a life changing event. The body undergoes major changes. For most women, this is a happy and positive experience, but for some there may be considerable discomfort or even ill-health while pregnant. If you feel depressed or anxious about yourself, your pregnancy or your baby, please tell your midwife or doctor, as they will be able to offer support.
After your baby's birth
If your weight is more than 120kgs, you will remain on Delivery Suite until you are fully mobile.
This is a safety precaution.
Breastfeeding
Breastfeeding has lots of benefits to both you and your baby. Your midwife and health visitor will have discussed these benefits with you during your pregnancy.
- Breastfeeding can help prevent your baby becoming overweight in childhood and as an adult.
- It can also help manage your weight.
You will be given support with breastfeeding during your hospital stay. When you are discharged from hospital, further support is available from your Community Midwife and our Early Breastfeeding Support Service.
Wound care
If you have a high BMI, there are increased risks of wound infection, wound breakdown and delayed wound healing. Delayed wound healing could last for weeks or months, depending on the severity:
If your BMI is more than 40, and you have had a caesarean section, your wound will be covered with a special dressing. This is a small pump-operated dressing that will cover your wound for five days; this has been shown to greatly reduce the risk of wound infection. Once the dressing has been removed it is important to ensure the wound is kept clean and dry. We recommend you do not wear underwear that may rub against your scar, as this may cause redness and breakdown of your scar.
During your hospital stay and during postnatal visits, the midwife will check your scar to ensure there are no signs of a wound infection or breakdown. If at any time you are worried about your scar, please contact the unit.
If you have had a vaginal delivery with stitches, it is important that you keep the area as clean and dry as possible, by regularly changing sanitary pads. We recommend you use Maternity pads during the early postnatal period.
Blood clots
- You may also need to have a course of blood-thinning injections (Enoxaparin) after delivery of your baby; this is to reduce your risk of developing blood clots. You will be asked to continue with these when you go home. You (or your partner) will be shown how to do this.
- You will be encouraged to move around as soon as possible after the birth and drink plenty of fluids. We will also give you some stockings to wear to further reduce the risk of blood clots.
- If your BMI is above 35 you should avoid the Combined Oral Contraceptive Pill, as this increases your risk of Deep Veined Thrombosis. Speak to your GP or Family Planning Clinic regarding alternative forms of contraception.
Future pregnancies
- It is advisable to try and reduce your weight after the birth of your baby and before planning any future pregnancies. Your GP may be able to offer further advice and referral to a Dietician.
- It is recommended you start taking folic acid once a day at least one month prior to becoming pregnant, and until the 13th week of pregnancy.
Further information:
https://
https://
https://
Image credit:
Eatwell Guide.
Crown copyright. OHID in association with the Welsh government, Food Standards Scotland and the Food Standards Agency in Northern Ireland.
George Eliot Hospital is a smoke free environment. For help and advice to stop smoking you can call the national helpline on 0300 123 1044 or visit https://
Copyright
Except where otherwise noted, this item is licensed under the CC BY license (https://
If you are a rights holder and are concerned that you have found material on our patient information resources website, for which you have not given permission, or is not covered by a limitation or exception in national law, please contact us using the Feedback form providing your contact information and full details of the material.